On December 1, 2020 the Centers for Medicare & Medicaid Services (CMS) issued a Final Rule that updated policy changes related to the Medicare payments under the Physician Fee Schedule on and after January 1, 2021.1 The changes for evaluation and management (E/M) codes impact physician documentation, proper selection of the E/M level, and the associated work relative value units (wRVUs). Below we highlight changes to the Final Rule that will impact physician employment agreements for 2021.
First, CMS adopted the American Medical Association (AMA) guidance for current procedural terminology (CPT) coding effective January 1, 2021. The outpatient E/M codes historically have been selected based on the history and review of systems documented by the provider. Now the review of the number of body systems or areas reviewed and examined under the history and examination will no longer apply. The history and physical components will be documented if clinically appropriate. However, the level of an E/M visit will depend upon the medical decision-making, or the time spent by the practitioner during the visit.
Medical Decision Making (MDM) falls into four categories: straightforward, low, moderate, and high. MDM is based on the number and complexity of the problems addressed at the time of the visit, the amount and/or complexity of data to be reviewed and analyzed, and the risk of complications, morbidity, and/or mortality of patient management decisions made at the visit, associated with the patient’s problem(s), the diagnostic procedure(s), treatment(s).2 The time spent by the practitioner means “the total time on the date of the encounter. It includes both the face-to-face and non-face-to-face time personally spent by the physician and/or other qualified health care professional(s) on the day of the encounter (includes time in activities that require the physician or other qualified health care professional and does not include time in activities normally performed by clinical staff)”.3 Depending on the MDM and the time expended during the encounter, the proper E/M code should be selected by the provider.
If there are prolonged visits that exceed the normal times for E/M new patient and established patients, CMS adopted an additional code for billing for each fifteen (15) minutes in excess of the E/M code time limits. CMS also approved the HCPCS G2212 code for additional time in excess of the top end of the E/M visit time limitation. Further, CMS approved a HCPCS G2211 code to capture complex patient visits. Therefore, CMS attempted to design a CPT Code methodology that it believes “will further our ongoing effort to reduce administrative burden, improve payment accuracy, and update the O/O E/M visit code set to better reflect the current practice of medicine”.4
With the changes to the E/M codes, new values for CPT codes 99202 through 99215 were determined and CMS assigned RVUs to the codes, as well as the new HCPCS code G2211 and G2212. The new values are as follows:
Summary of Codes and Work RVUs Finalized in the CY 2020 PFS Final Rule for CY 20215
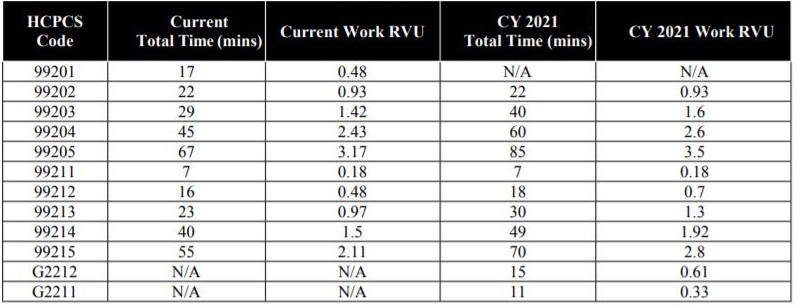
All of the wRVU rates increased for the E/M codes which directly impact primary care and physician-based practices. In addition to the increase in the wRVU rates for the E/M codes, CMS also supported increases in value for the following types of services:
- End-stage renal disease monthly capitation payment (ESRD MCP)
- Transitional care management (TCM)
- Maternity
- Cognitive impairment assessment and care planning
- Annual wellness visits (AWV) and initial preventive physical exam (IPPE)
- Emergency department (ED) visits
- Therapy evaluations
- Certain behavioral healthcare services
Therefore, as Hospital and Health Systems consider employment or contractual arrangements that involve any of the above referenced services, the Hospital or Health System should evaluate all compensation arrangements that utilize wRVUs as part of the compensation model.
While the wRVU-assigned values are increasing for E/M visits and certain services, the conversion factor rate for RVUs for 2021 will decrease by $3.68. Specifically, the conversion rate for the 2021 Year will be $32.41 for the RVU. This change is intended to conform to the budget neutrality adjustment required by law.
Considering the increases in wRVU values with a decrease in the RVU conversion amount, if the hospital or health system employs physicians with a compensation model based upon wRVUs, it is important to evaluate and potentially modify the physicians’ employment contracts for 2021. For example, if a hospital or health system pays a physician $300,000.00 annual base salary and the physician’s personal productivity exceeds 6000 wRVUs per year (minimum wRVU threshold) then he or she receives as a productivity bonus of $50.00 per wRVU performed in excess of the minimum wRVU threshold. Under this example, the physician will reach the minimum wRVU threshold earlier during the year and will likely receive higher productivity bonus payments than in previous years. Likewise, if the physician’s compensation is based solely upon wRVUs, the physician’s total compensation will be higher in 2021, if his or her productivity is similar to prior years. However, the reimbursement may potentially decline, leading to an increased loss to the hospital or health system when the physician’s compensation increases, but the reimbursement decreases. Therefore, hospital or health system employers should perform a CPT code analysis of its employed physicians, analyze the receipts for the physicians and confirm if the projected compensation for 2021 remains consistent with fair market value standards and is commercially reasonable. The total projected compensation amount may exceed fair market value standards and it is recommended to amend the employment agreements to ensure the compensation model remains consistent with fair market value standards and is commercially reasonable.
It is important to note that the majority of the CMS CPT code increases are limited to E/M codes that are performed by physicians in the outpatient physician practice setting. In order to offset the potential increases, CMS also provided for decreases in values related to facility procedures and specialty services in the facility setting. Therefore, the hospital and health systems should also evaluate all contracts for specialty services and hospital based services. If the hospital or health system maintains contracts with specialists or hospital based providers, the reimbursement may decline and the compensation arrangements may require adjustment to avoid financial losses to the hospitals or health systems.
In conclusion, physician compensation arrangements should be evaluated based upon historical performance applying the new 2021 CPT and wRVU changes to ensure the agreements remain in compliance with the fair market value standards and are commercially reasonable in light of the financial impact.
If you have any questions about this legal update, please contact a member of the MMM healthcare group.

